Health and Wellness
STD Testing: When, How, Where, and What to Expect with STI Screening

When thinking about sex, you probably would rather focus on how good it feels and getting more of it, and less about sexually transmitted infections (STIs or STDs). But the reality is: they happen. There are an estimated 26 million new cases in the United States each year—and part of taking care of ourselves and our partners is getting tested for STIs.
What that number means is that STIs are quite common, so if you think you might have one, you’re not alone. Getting tested for an STD can seem scary, embarrassing, or difficult, but STI tests are easy to find, and you can do them at a clinic, a doctor’s office, or even in your own living room. They’re also often free or covered by insurance and not hard to do, sometimes as simple as pricking your finger or peeing in a cup.
What is STI Testing and How Do STD Tests Work?
STI testing works by taking samples of your blood, urine, saliva, or genital secretions and checking them for bacteria that cause STDs such as chlamydia, gonorrhea, trichomoniasis, syphilis or the viruses that cause HPV, herpes, hepatitis or HIV. Many STIs can have no symptoms, so testing is the only way to know for sure if you have one.
This article will answer your questions about where to find STI tests, the ease and importance of taking them, plus how often you should get tested. If you’re looking for other information, read more about common STI symptoms as well as using condoms to prevent STIs.
When Should I Get an STD Test?
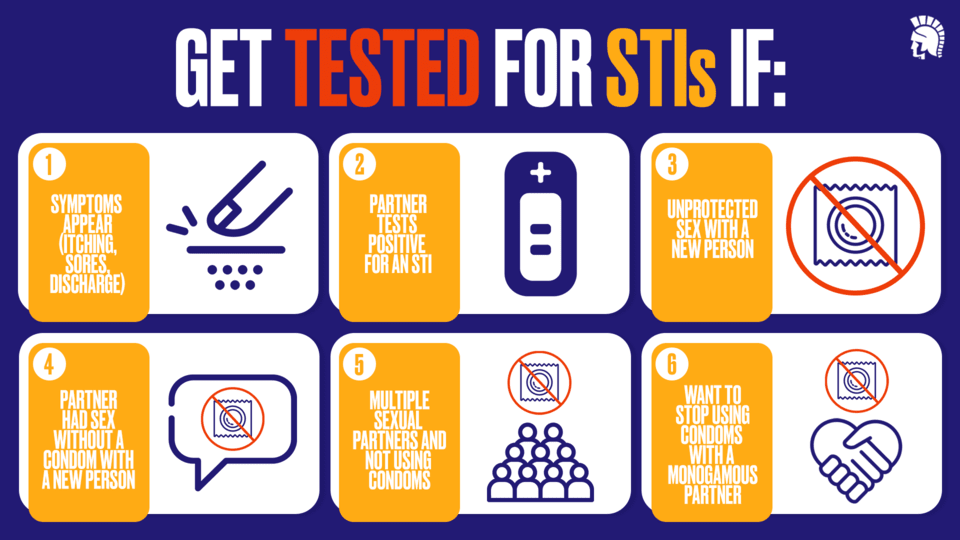
If you’re sexually active, especially with multiple partners, STI screening should be part of your routine every 3-6 months. Get an STD test when any of the following occur:
You discover symptoms, including sores, bumps, rashes, or unusual discharge
Any of your partners test positive for an STI
You had unprotected sex with someone you don’t know
Your partner has had sex without a condom with someone whose STI status is unknown
You have multiple sexual partners and are not using condoms
You’re planning to stop using condoms with a monogamous partner
Where Can I Get Tested for STIs?
STI tests are readily available. At-home tests for some STIs can typically be found at your local CVS, Walgreens or another drug store. Or, you can choose to order an STI test online and make an appointment with Telehealth for a discreet option.
There are also a lot of options for in-person testing, many of which are free. These may include:
Health departments
College student health centers
Health clinics
Organizations like Planned Parenthood
Your primary care doctor or OB/GYN
The CDC has resources to help you find the closest place to get tested.
Can I Test for STIs at Home?
There are at-home STI tests available for most common STDs, including HIV, gonorrhea, chlamydia, syphilis, trichomoniasis, and hepatitis-C. You can choose a “full-panel” test or tests that look for a specific STI. Testing yourself at home is convenient (you can do the whole thing in your pajamas), private, and the results are generally accurate. It is important to follow instructions when conducting at-home STI tests carefully to ensure your samples can be used.
Local health departments may offer self-testing kits for free, or you can buy them online or in a pharmacy using HSA/FSA funds or conventional payment. Make sure to confirm your health plan includes HSA/FSA eligibility before proceeding to purchase.
At-home tests are good for STI screening, but if you have symptoms or get a positive result, see your provider who can verify results, recommend any other tests, and prescribe treatment.
What’s the Difference between STI Screening and STI Testing?
STI testing is done when people have symptoms while STI screening is for people who just want to know, but the procedures for testing and screening are the same. Everyone who is sexually active should be screened for STIs regularly, depending on your risk factors. Anyone who has symptoms should get tested right away. Read on for more specific recommendations.
How Often Should I Get Screened for STIs?
STI screening recommendations are based on your age and risk factors. Everyone should be screened for HIV at least once. Sexually active women age 25 and under, men who have sex with men, and anyone who receives anal penetration should be screened for chlamydia and gonorrhea every 3 to 6 months. Pregnant people need to be screened for multiple STIs for their own health and their baby’s. The CDC does not recommend screening for herpes for people who do not have symptoms.
Recommended STI screenings are also based on your behavior. People with multiple partners may STD screening or testing before having sex with a new partner. And anyone who engages in other risky behavior—like sharing needles for drug use or having anal sex—should get screened every six months or at least once a year for HIV and Hepatitis C.
How Often Should I Get Screened for HPV?
If you’ve had the HPV vaccine as a teenager to prevent HPV-related cancers, then HPV testing is not recommended. If you’re unvaccinated or older than 26 and have a cervix, the CDC recommendation is screening for HPV every 5 years and a Pap smear test every 3 years.
The CDC does not recommend HPV screening for men, but some healthcare providers offer anal Pap tests for men who receive anal sex or are at greater risk of cancer. Of course, if you have any symptoms of genital warts, get tested right away.
If you’re under age 26 and not vaccinated against HPV, getting the vaccine is a good way to prevent HPV and HPV-related cancers. Wearing a condom helps protect against HPV, as well as other STIs.
What is Included in a Full STD Panel?
Which specific STI tests are included in a basic, comprehensive, or “full panel” STD test may vary depending on your provider, but all STD panels typically include the most common STIs: chlamydia, gonorrhea, syphilis, Hepatitis B and C, plus HIV. Some STI tests are more limited, while others may also test for herpes or trichomoniasis, among other STIs. Ask your provider or check the test kit you’re using to know which STIs are included.
It is important to be honest with your provider about your sexual history and any symptoms you have. The more they know, the better they can be at choosing which tests you need. If you are going the at-home testing route, you might want to find the most inclusive panel so you can test for a wider range of STIs.
How Long Does It Take to Do an STD Test and How Long Do STI Results Take?
Obtaining the samples from an STI test takes just a few minutes, regardless of whether you’re taking a rapid at-home STI test or getting tested at a clinic or doctor’s office. Newly approved Rapid STI tests can provide results for most STIs, including HIV, in about 30 minutes, while traditional lab tests usually take 1-3 days for results to come back. Some tests can take longer (up to 14 days) for confirmed results.
Ultimately, there’s not an easy or straightforward answer that applies to all STI tests. While sample collection is simple and fast, getting results can take minutes or weeks, depending on the test. If you think you might have an STI while waiting for test results, be sure to wear a condom when having sex to prevent possible transmission.
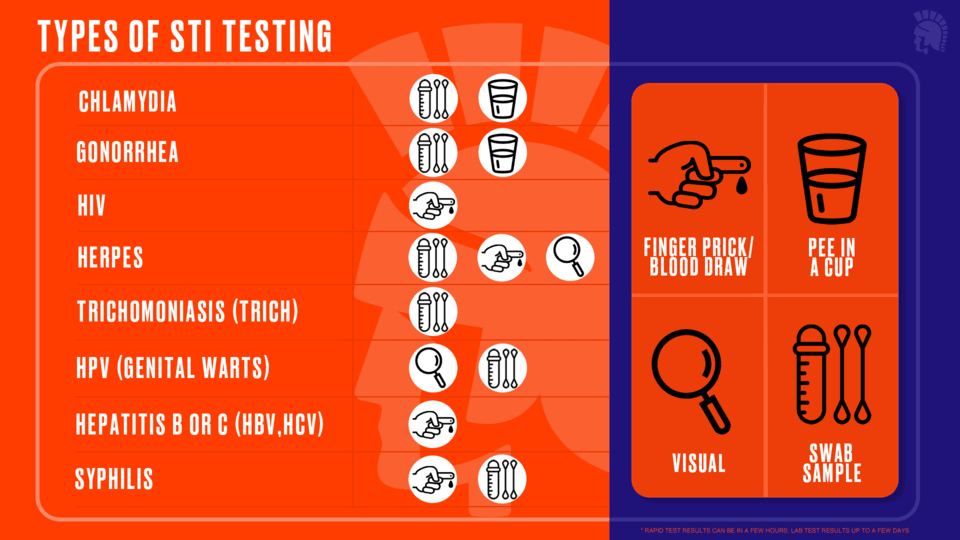
Types of STI Tests
When taking an STI test or STD screening, you may need to provide a sample of blood or urine or take a swab of your mouth or genitals. Which type of test is needed depends on what STIs you are testing for and whether you have symptoms.
Urine STI tests
These tests are pretty easy. You pee in a cup and your urine is tested for bacterial infections like gonorrhea, chlamydia, and trichomoniasis.
Swab tests for STDs
These tests use a cotton swab like the ones you’re used to from throat cultures or Covid-19 tests to gather samples from the urethra (the hole where urine exits), the vagina, the cervix (the bottom of the uterus), the throat, or the anus. Some tests let you do your own swabbing which might be more comfortable for some people.
Blood tests to check for STIs
For these tests, a health care provider might take a blood sample from your vein or might prick your finger. Blood tests can be used to check for syphilis, Hepatitis-C, and HIV.
Physical exam at a doctor or clinic
If you have symptoms, a health care provider will look for sores, rashes, discharge, swollen glands or other physical signs to help diagnose an STD and decide which STI tests you need. The doctor may scrape cells from a sore to confirm a visual diagnosis.
What is a Rapid STI Test?
A rapid STI test is a newly FDA-approved PCR test for gonorrhea, chlamydia trichomoniasis, or hepatitis-C, with the results available in 28 minutes. There are also rapid HIV antibody tests that provide results in about 20 mins.
These rapid STI tests use urine and saliva samples, finger-pricks, or swabs of the urethra, vagina, or cervix to check for the targeted STIs. Most Rapid STI tests are self-administered, and they can be an easy, discreet, and convenient way to know your status right away.
However, rapid STI tests are not as quite as accurate as lab tests, so it is possible to get a false negative, especially if you did the test yourself. If you test positive with a Rapid STI test, make a Telehealth appointment, visit a health clinic or see your healthcare provider right away to get treatment and any further tests.
Can You Test Negative for an STI and Still Have It?
It is possible to get a false negative on an STI test due to problems with the test, the way the sample was collected, or if you tested too soon after exposure. Some STIs, like gonorrhea, chlamydia and syphilis, may show up within days or a few weeks. Others, such as HIV, may take up to 3 months before showing up on a test.
The time between getting infected with an STD and it showing up on a test is sometimes called the window period. If you think you might have tested during the window period, consider using condoms until you can take the test again to confirm the results.
Can You Have Sex if You Have an STI?
Whether you can have sex with an STI depends on the STI, the treatment, and your symptoms. Most health care providers will tell you not to have sex if you have a rash, discharge or sores, especially if the sores won’t be covered by a condom. Sex might cause pain to you and be risky for a partner.
For STIs that can be cured with antibiotics (like gonorrhea or chlamydia), it is usually best to wait about 7 days until all partners have finished treatment to make sure you don’t keep passing germs back and forth. If you do decide to have sex before that point, it’s very important to wear a condom.
Other STIs can’t be cured, but that does not mean you cannot have sex. If you have herpes, you should avoid sex when you have an active infection, which may appear as sores on your genitals or mouth. People with herpes often say they can feel an outbreak coming. In this case, be sure to use a condom for oral or penetrative sex. You can also take antiviral medications to prevent outbreaks, which lets you enjoy a more active sex life.
If you are living with HIV, you can take medication that suppresses the virus in the body to the point that it’s undetectable in a blood test. When you are undetectable, you can’t transmit the virus to a partner during sex. Still, you should use a condom if there’s a gap in your consumption of HIV meds, as well as to help protect against other STIs.
An STI is not the signal that your sex life is over, but it might mean you have to take a quick break while you get treated. It’s also a good reminder to talk to your partner about prevention.
If you have an STI, communicate with your partner and make a collective decision about your comfort level in having sex. Should you decide to engage in sexual activity, make sure to use a condom.
Regular STI Screening Helps You Stay Protected
Public health experts often say that STI testing is a form of prevention. What they mean is that once you know you have an infection you can take the right steps to prevent giving it to your partners, which not only protects them but protects anyone else they might have sex with. Testing and treatment can stop the cycle and contain the spread of STIs.
Of course, avoiding STIs entirely is the ultimate goal, which is why prevention methods like condoms and vaccines are so important. Trojan™ condoms, like BareSkin™ Raw™ and Magnum™ Raw™ make it feel as though you’re hitting it like it’s raw while still helping you stay protected so you can have safer and more regular sex.